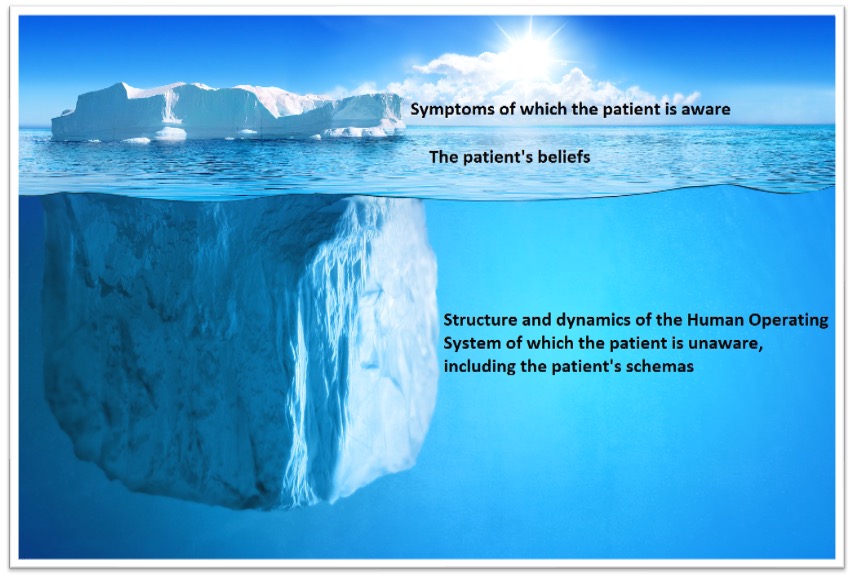
Such symptoms (e.g. depression, anxiety, trauma, pain) are often experienced by the sufferer as a foreign agent that has attacked them – like the psychological equivalent of a viral/bacterial infection that can be fought and killed. However, in reality mental health and functional disorders (such as IBS and other Disorders of Gut-Brain Interaction) are never like that: symptoms and conditions are always and necessarily a consequence of the dynamic interaction of psychological, neurological, physiological and environmental factors taking place within the HOS – that is the body, brain and mind of the individual in relation to their environment (including other people and the totality of the individual’s life circumstances).
It can be understood from the above how badly the predominant symptom-based model of mental health fails people. It denies them the opportunity to arrive at a deeper understanding of what is giving rise to their symptoms, the full range of practical steps they can take to get better and avoid relapse, and how they can continue to enhance their mental health, happiness and wellbeing throughout their life.
Symptom reduction misses strength-based opportunities
A symptom reduction approach to mental health also misses countless opportunities to maximise personal strengths and positive life opportunities that could enhance the patient’s life. Mental wellness is not just the absence of symptoms but rather the presence of qualities and skills that enable the patient to navigate through their life circumstances, take advantage of life opportunities and develop meaningful relationships in all areas of life.
We are collaborating with wellbeing experts including Professor Sarah Stewart-Brown who developed the WEMWBS (Warwick-Edinburgh Mental Wellbeing Scales) to address the deficiencies of existing mental health scales (e.g. GAD-7 for anxiety and PHQ-9 for depression) which focus only on symptoms. Professor Stewart-Brown was motivated to develop this scale having recognised that existing scales failed to capture wellbeing and were inadequate for providing appropriate measures and recognition of interventions which improved wellbeing.
The 14 questions of WEMWBS serve as an initial intervention. By inviting the patient to consider their wellbeing across 14 criteria they are invited to enter into a process of self-enquiry and self-awareness on how to enhance their wellbeing in each area – this in turn, will allow them to recognise opportunities to do so. MindLife sees considerable scope for developing upon the existing strengths of WEMWBS by creating hybrid/blended interventions that support users to enhance their wellbeing across all 14 dimensions.
Symptom reduction approaches are insufficiently effective in terms of symptom reduction
Symptom reduction approaches are not even sufficiently effective on their own terms – that is in terms of symptom reduction. The dominant therapy method is CBT, which is a conversation between the “logical mind” of the therapist and the “logical mind” of the patient/client. In CBT the therapist is explaining to the patient how to improve their way of thinking and behaviour.
However, our thoughts and emotions are created by our ‘HOS’ and our autonomic nervous system. For many conditions and patients CBT, which does not consider the HOS, is not effective. We are integrating a variety of methods which are more effective for specific conditions, patient’s needs and preferences. For example, PTSD is treated in the NHS using trauma-focused CBT, or EMDR, which require up to 20 sessions with specialised therapists. Yet 60% still don’t recover!
We have researched a much more effective and scalable method in which most patients recover in less than 5 sessions. The NHS also lacks effective treatments for IBS. The NHS states about IBS “it’s usually a lifelong problem. It can be very frustrating and can have a big impact on your everyday life”. We developed an effective treatment for IBS that helped most patients (proven in RCT).
Moving beyond the symptom-centric paradigm
We are aware of a number of companies within the digital wellbeing space that are seeking to utilise AI/Machine Learning analysis of data in order to improve treatment (e.g. IESO) and others that employ biofeedback to guide treatment (e.g Graymatters.health). However, they do so within the framework of the predominant reductionistic symptom-centric paradigm and the therapies associated with it. The symptom-centric paradigm that they are working within imposes a glass ceiling upon the level and types of benefit that such companies can offer to their customers that no amount of investment funding or sophisticated AI will enable them to transcend.
Concurrently, a number of well-respected and deeply insightful psychologists and psychotherapists are developing psychotherapeutic methodologies (e.g. Interpersonal Neurobiology – IPNB) that provide a strengths-based approach to mental health. However, these methods haven’t been computerised yet.
We’re collaborating with experts who’re developing/using such methods and enhancing them with computerised therapy options and AI. This makes them scalable and cost-effective – vastly increasing their potential reach and usefulness. Furthermore, through our computerised recommendations systems we’ll be able to offer each client/user the most effective solutions according to their needs and preferences.